Chronicling the process of providing integrated primary care and behavioral health care
Thursday, October 31, 2013
Tuesday, October 29, 2013
Saturday, October 26, 2013
Scribble Drawing Class
Today's art therapy class was about scribble drawing. Clients were given the following instruction by the art therapy intern: "Start by creating a scribble with eyes closed or open. Open your eyes and look at what is on the page. See if you can see any concrete images in your scribble. Finish the drawing by coloring in shapes or adding new lines to create a finished drawing. When you are done, give the drawing a title. Share with the rest of the group how it made you feel. Were there any surprises or images that emerged?"
One client had a hard time starting the scribble and wanted to draw with eyes open. The art therapy intern demonstrated how she does a scribble drawing and then the client was able to do this on his own. She reported, "he was very excited to be in the group..." He titled his drawing, “Mountain Park Holyoke” because it reminded him of the colors and rides of Mountain Park. "It seemed like a happy memory for him," concluded the art therapy intern.
Thursday, October 24, 2013
Baseline Evaluation
Provided below is information about baseline data (and preliminary six-month
analysis) on the 85 patients currently enrolled in the CHD Health &
Wellness integrated services program. With respect to demographics, the group
is comprised of approximately 50% under age 45 and 50% over age 45. Sixty
percent of the group is female and 38% of the group is male, with 2% reportedly
trangendered. Half of the group is Caucasian and one-quarter each is Puerto
Rican and African American.
As for functioning, 45% either agree or strongly agree that they are in "excellent health, very good or just good." CHD Health & Wellness patients report low rates of problem use with alcohol and a range of illicit drugs. Less than half of those enrolled report smoking tobacco less than weekly.
No patients report being homeless in the past 30 days. Ninety-five percent had not been admitted to a psychiatric hospital. In the past 30 days, 98% had not been admitted to a detoxification unit, none had been to jail, and 93% had not been admitted to an emergency room.
Two-thirds patients are currently permanently housed. Those who are not housed, include those living in someone else's house, in transitional living, or acute care.
With respect to social connectedness, over 70% of patients report being satisfied with their friendships; 78% have people with whom they do enjoyable things.
Health measures collected at baseline indicate that enrolled patients are at risk. The high rates of risk are for the following indicators: CO measure (46%), weight (4% underweight and 87% obese at risk). One-hundred percent of the enrollees are at risk regarding waist circumference. In addition, according to blood draw results, 78% of the population being served tested at risk for the indicator A1C and 43% tested at risk regarding Triglycerides.
In the following section, outcomes at six-months for the 14 patients, who have matched intake and six-month data, are examined. There was a 14% increase in the number of patients who reported their overall health to be good or better than good at the six-month data point. Those who reported not being bothered by symptoms fell by 29%.
There were improvements in mental health symptoms having to do with feelings of hopelessness (30%), depression (50%), feeling like everything is an effort (25%), and worthlessness (25%). The number of patients feeling little or no nervousness, or restlessness dropped by 40% and 25%, respectively, at the six-month data point in the CHD Health & Wellness program.
There were improvements in the number of patients reporting less than weekly use of cannabis (7%) and prescription opioids (7%) and no change was noted in the number of patients using alcohol less than weekly.
Patients continue to report not being homeless at the six-month data point. There were no admissions to psychiatric hospitals, detoxification units, or incarceration same as program entry. The number of patients receiving school or job training increased by (300%) at the six-month data point yet there was a drop of 40% in those employed at six months.
Source: CAR, Evaluation Report, October 21, 2013
As for functioning, 45% either agree or strongly agree that they are in "excellent health, very good or just good." CHD Health & Wellness patients report low rates of problem use with alcohol and a range of illicit drugs. Less than half of those enrolled report smoking tobacco less than weekly.
No patients report being homeless in the past 30 days. Ninety-five percent had not been admitted to a psychiatric hospital. In the past 30 days, 98% had not been admitted to a detoxification unit, none had been to jail, and 93% had not been admitted to an emergency room.
Two-thirds patients are currently permanently housed. Those who are not housed, include those living in someone else's house, in transitional living, or acute care.
With respect to social connectedness, over 70% of patients report being satisfied with their friendships; 78% have people with whom they do enjoyable things.
Health measures collected at baseline indicate that enrolled patients are at risk. The high rates of risk are for the following indicators: CO measure (46%), weight (4% underweight and 87% obese at risk). One-hundred percent of the enrollees are at risk regarding waist circumference. In addition, according to blood draw results, 78% of the population being served tested at risk for the indicator A1C and 43% tested at risk regarding Triglycerides.
In the following section, outcomes at six-months for the 14 patients, who have matched intake and six-month data, are examined. There was a 14% increase in the number of patients who reported their overall health to be good or better than good at the six-month data point. Those who reported not being bothered by symptoms fell by 29%.
There were improvements in mental health symptoms having to do with feelings of hopelessness (30%), depression (50%), feeling like everything is an effort (25%), and worthlessness (25%). The number of patients feeling little or no nervousness, or restlessness dropped by 40% and 25%, respectively, at the six-month data point in the CHD Health & Wellness program.
There were improvements in the number of patients reporting less than weekly use of cannabis (7%) and prescription opioids (7%) and no change was noted in the number of patients using alcohol less than weekly.
Patients continue to report not being homeless at the six-month data point. There were no admissions to psychiatric hospitals, detoxification units, or incarceration same as program entry. The number of patients receiving school or job training increased by (300%) at the six-month data point yet there was a drop of 40% in those employed at six months.
Source: CAR, Evaluation Report, October 21, 2013
Tuesday, October 22, 2013
Meeting Meaningful Use Standards
Meaningful use
standards. Our two FQHC partners implemented
their EMRs, OCHIN-EPIC, with "go live" dates of March 1, 2013 and
July 16, 2013, respectively. The Practice Teams are aware of the need to
achieve meaningful use and a timeline is in place that should support the
achievement of MU by December 2013.
The first FQHC is at the
second year of Meaningful Use. This means that its providers use electronic
prescribing for more than 40% of prescriptions, assess smoking status in more
than 50% of patients, generate a visit summary for patients greater than 50% of
the time and generate reminders for visits greater than 20% of the time.
The second FQHC reports that it is
currently at Level 2 of the NCQA Primary Care Medical Home (PCMH) and has built
into the EMR planning, the attainment of Levels 3 and 4 of PCMH, once staff are
fully trained and system is fully implemented. CHC is already using
e-prescribing (and does so for more than 40% of prescriptions), tobacco use is
assessed for all patients over the age of 12 (and tobacco cessation counseling
is available internally), visit summaries are generated in our current paper
records (more than 50%), and reminders go out via phone for more than 70% of
our patients. The FQHC purchased OCHIN/EPIC. EPIC is the product and OCHIN is
the third party seller of the product. Staffs are currently being trained on
the use of the product. Discussions are ongoing with CHD Health & Wellness
regarding the interface between our EHR and their behavioral health electronic
records.
CHD Health & Wellness had already planned to
transition to a new electronic medical record (EMR) system called Profiler in
advance of award of this grant. As such, other than staff meetings between IT
staffs of CHD and the health centers, no additional costs for integration of
the systems have been incurred as of yet.
Barriers to Accomplishments. Given constraints
of the participating site’s EMRs, there are challenges to integrating the
systems which require staff time to facilitate workarounds.
Actions to Overcome
Difficulties. In an attempt to reduce as many workarounds as possible,
considerable time and effort has been given to mapping out the workflows for
staff so that administrative efficiencies may be realized. The original
workflows continue to be updated by staff as the project unfolds. Recently, CHD
Health & Wellness project manager, Dr. Higgins, began using the workflows
as the basis for quality improvement meetings with care managers. During these
meetings, staffs continue to identify ways in which to make data entry and EMR
use more efficient. Dr. Higgins is also using PDSA analysis to improve
efficiency and hopes to supply project funder with her findings at a later
time.
CHD Health & Wellness's external evaluation team has developed
a dashboard to support the regularly scheduled extraction of data from multiple
systems. In July, 2013, the evaluator implemented the first quality assurance
process to analyze and improve data extraction processes.
Sunday, October 20, 2013
Integration in Practice
"I got word this afternoon that [one of CHD Health & Wellness's] patient's potassium levels were at a critical level," said our care manager. "The clinic nurse got a call from the lab. Meanwhile the endocrinologist called the [FQHC] to alert staffs after directing the patient to the ER. The RN who works with CHD Health & Wellness's PCP called over to CHD Health & Wellness to inform us (at the very same time I was notifying the [FQHC] via the EMR). I then faxed over to the RN the lab report that came to us (CHD Health & Wellness APRN had ordered the testing). Integration services at work!" proudly exclaimed the care manager.
This description of the complex work being provided by CHD Health & Wellness is a prime example of a truly integrated system. Not only are patients more likely to get the most appropriate care needed for their conditions, there is an increased likelihood that clients will willingly obtain medical care due to the increased familiarity of the integrated services team and the proximity of services being provided. For CHD Health & Wellness clients, onsite primary care demystifies the process of obtaining medical care. And as typified by the example provided by CHD Health & Wellness case manager, all team players can communicate with greater ease.
This description of the complex work being provided by CHD Health & Wellness is a prime example of a truly integrated system. Not only are patients more likely to get the most appropriate care needed for their conditions, there is an increased likelihood that clients will willingly obtain medical care due to the increased familiarity of the integrated services team and the proximity of services being provided. For CHD Health & Wellness clients, onsite primary care demystifies the process of obtaining medical care. And as typified by the example provided by CHD Health & Wellness case manager, all team players can communicate with greater ease.
Friday, October 18, 2013
Thursday, October 17, 2013
"Walking Machine"
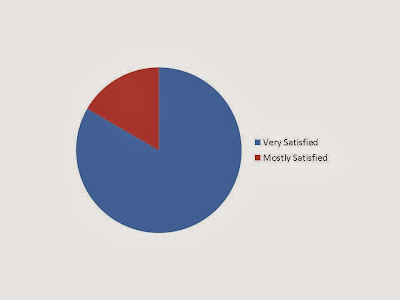
Satisfaction Survey Results
Well, the results are in! Six CHD Health & Wellness enrollees have completed their anonymous six-month satisfaction questionnaires. Results indicate that all six enrollees are very satisfied with the majority of the program. For instance, they are very satisfied with their primary care providers, their care managers, their overall medical care, and their individual wellness programs. One client indicates that s/he is only mostly satisfied with the timeliness of her/his visits, the variety of wellness programming and the facilities, or physical space in which the primary care visits are conducted. All in all, CHD Health & Wellness staff is pleased with the results of this survey of a handful of enrollees who have reached the six-month mark. But, they also realize there is much work yet to be done.
(Source: Survey completed by six enrollees who have been enrolled for at least 6 months)
Sustaining Wellness Programs
Wellness-related programming. Our care managers (with the assistance of the advisory group) have implemented the following wellness programs: healthy eating and cooking classes, yoga, Zumba, Latin and ballroom dance, “Walk with a Doc,” therapeutic laughter and writing groups, chronic disease self-management program, gardening club (for growing herbs with which to cook), diabetes management and cognitive/sensory processing workshops.
Barriers to accomplishments. One barrier to implementing the wellness programs is that they are non-billable and therefore harder to make sustainable.
Actions to overcome difficulties. In order to make the wellness programs sustainable, it is the goal of our integrated services program to have these programmatic offerings be budget neutral. However, fundraisers for the wellness programs are also planned as a way to generate revenue needed to fund these non-billable programs. Fundraisers included a dine-out for a cause event at a local restaurant and a 5K race/walk. All funds generated from these events are tracked separately and earmarked for underwriting wellness programs. Another source of wellness programming revenue is regularly provided by a private donor.
Care Managers: A New Professional Role
Care managers in integrated service programs function in a hybrid fashion combining community mental health case management and medical case management. This hybrid form of case management involves not only the coordination of community services for seriously mentally ill clients but also a collaborative process with medical providers to facilitate recommended treatment plans to assure appropriate medical care is provided. As is the case with all types of case management, the care managers’ tasks include assessment of need, care planning, implementation and regular review. Their case management is clinical, or therapeutic, in nature, requiring that they establish therapeutic relationships with their clients and that they are actively involved in their clinical care. They also evaluate clients’ medical conditions, coordinate medical resources, communicate healthcare needs to clients, monitor their progress and promote cost-effective care.
Love Your Body
In honor of “Love Your Body Day”, which is the campaign of the National Organization for Women (NOW), our new CHD Health & Wellness art therapy intern led a group of clients in a class designed to create images of oneself, noting what each of them liked (or better yet, loved) about themself. The images were hung on a newly decorated bulletin board at our clinic. Clients were encouraged to keep adding new images to the board during the month of October. Upon seeing the hearts all over the board, one client inquired, “What is this; Valentine’s Day?” This provided a perfect opportunity for our intern to explain what the significance of the day was and what clients were in the process of doing.
According to NOW, ‘“Love Your Body Day” is a day when women of all sizes, colors, ages and abilities come together to celebrate self-acceptance and promote positive body image’.
Subscribe to:
Comments (Atom)